Plasma treatment benefits some COVID patients, NYU study finds
An NYU Grossman study found that transfusing blood plasma from recovered COVID-19 patients to COVID patients with preexisting conditions can improve the recovery process.
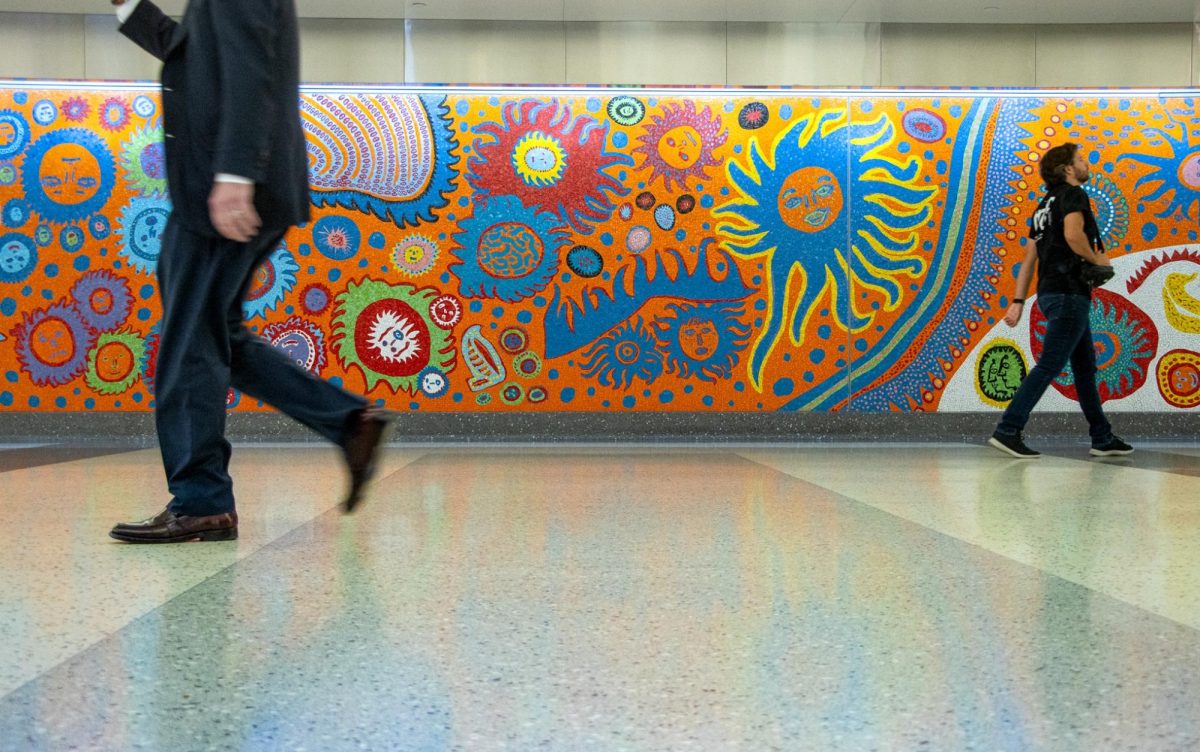
Convalescent plasma treatment can be effective in treating COVID-19 for selected patients, according to recent research from NYU’s Grossman School of Medicine. (Image via Wikimedia Commons)
February 16, 2022
Blood transfusions from people who previously recovered from COVID-19 have been found to improve the conditions of some currently infected with the virus, according to an NYU Grossman School of Medicine study published in late January. The Food and Drug Administration has considered the procedure experimental since authorizing the treatment for emergency use on hospitalized patients in August 2020.
The study analyzed 2,341 COVID-positive patients using eight randomized clinical trials from around the world. The treatment, known as convalescent plasma, appeared to have particularly strong benefits for specific groups: patients with mild symptoms and patients with preexisting conditions like diabetes, cardiovascular disease or pulmonary disease.
“This study represents an international collaboration across four continents and six countries, to pool information from studies in different patient populations to generate robust information about the possible benefits of convalescent plasma in treating COVID-19,” said Andrea Troxel, the study’s lead researcher and a Grossman professor. “Because the study was so large and the methods so rigorous, we were able to show that while it doesn’t benefit all patients, it may have positive effects in certain subgroups.”
Grossman professor Eva Petkova, another researcher on the study, said that patients with preexisting conditions are likely to benefit the most from the treatment since their ability to develop antibodies once infected with COVID-19 is compromised. The treatment is not as effective for all hospitalized COVID-19 patients.
Since the start of the pandemic, studies of convalescent plasma have led to mixed findings on its efficacy, prompting debate over whether the treatment should continue.
“It seems clear that there is a narrow window in which convalescent plasma might be effective,” Troxel said. “If patients are already hospitalized and severely ill, as in our study, it may be too late for convalescent plasma to work.”
After conducting the Grossman study, Petkov led a secondary study to develop a convalescent plasma treatment benefit calculator, which details the effectiveness of the procedure on different patients. The index allows clinicians to input their patients’ preexisting conditions and illnesses to determine their eligibility for the treatment.
“We derived a linear combination of patients’ baseline characteristics that indicates the expected benefit from treatment with convalescent plasma compared to treatment without convalescent plasma for individual patients,” Petkova said.
The secondary study analyzed 2,287 hospitalized COVID-19 patients to produce a set of guidelines for using the convalescent plasma as a treatment for infected patients. With Petkova’s study, doctors will have more information to decide whether convalescent plasma is appropriate for a given patient.
“If that probability is low, the clinician would probably choose a different treatment, but if the probability is high, they could decide to proceed to treat the patient with convalescent plasma,” Troxel said. “The new methods we developed are a model for future collaborations, especially in a crisis setting such as the COVID-19 pandemic.”
Contact Natalie Thomas at [email protected].