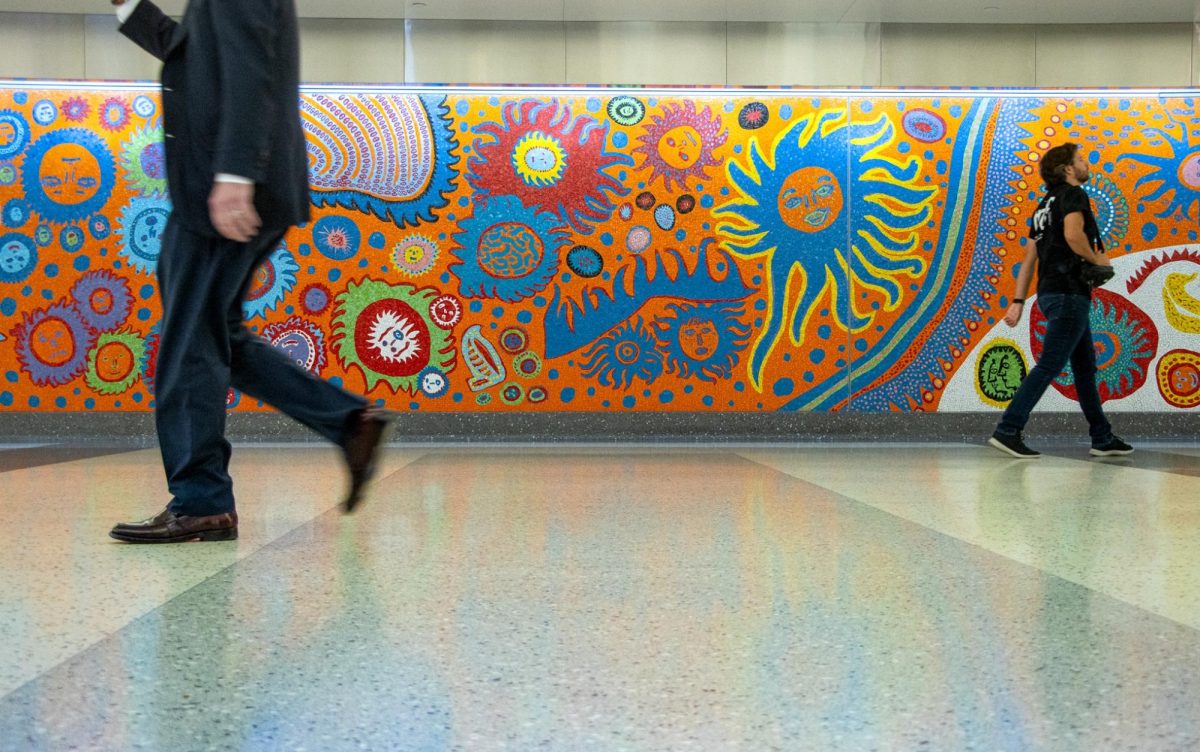
Kidney transplants between HIV-positive donors and recipients are just as safe as those from HIV-negative donors, researchers at NYU Langone Health found.
Prior to a study published last month, HIV-positive transplants were only performed under heavily monitored environments and for research purposes. After authors analyzed data from 198 transplants across 26 U.S. medical centers, they concluded that patients receiving kidneys from HIV-positive donors face similar side effects as those who received kidneys from donors without HIV — a practice that is currently under review by the U.S. Department of Health and Human Services.
Researchers told WSN that expanding the use of HIV-positive kidneys would make transplants more accessible and reduce backlog on waiting lists. Dorry Segev, an author of the study, said in an interview that he expects HIV-to-HIV transplants to be considered the standard of such care within a year.
“It opens the door for centers across the country who are interested in this from a clinical standpoint — not necessarily from a mechanistic biological standpoint — to start taking care of patients without the requirements that were in place for the research protocols,” said Segev, who is also the head of the Center for Surgical and Transplant Applied Research at NYU Langone.
Sapna Mehta, another author who has been studying kidney transplants from HIV-positive donors since at least 2019, said that NYU Langone could expand HIV-to-HIV heart and lung transplants within the next year. Mehta said the study aimed to inform HIV-positive candidates of their eligibility to donate organs.
“This will only be successful if people are aware that they can be a living kidney donor — even if they have HIV infection,” Mehta, an infectious diseases physician at the medical center, said.
The study compared one to three-year survival rates and transplant-related complications such as cancer, infection and organ rejection — all of which showed no substantial differences, regardless of whether the kidney tested positive for the disease. While HIV-positive transplants corresponded with an uptick in HIV blood counts, the authors said this was likely due to interruptions to patients’ pre-existing medications.
In 2019, Segev performed the first HIV kidney transplant in the United States at John Hopkins University after authoring the HIV Organ Policy Equity Act in 2013, which legalized clinical research on organ transplantation between HIV-positive donors and recipients. He said that under the HOPE Act, every kidney transplant saves Medicare about $500,000 because they are cheaper than keeping a patient on dialysis.
“It is actually a really cool celebration of what has happened,” Segev said. “The field of HIV evolved so much that today that aspect of the transplant is basically a non-issue.”
Contact Audrey Abrahams at [email protected].