Nurses’ insomnia, anxiety linked to pandemic stress
The group offered strategies for nurses to manage stress after exploring how COVID-19 exacerbated sleep deprivation, depression and anxiety among nurses.
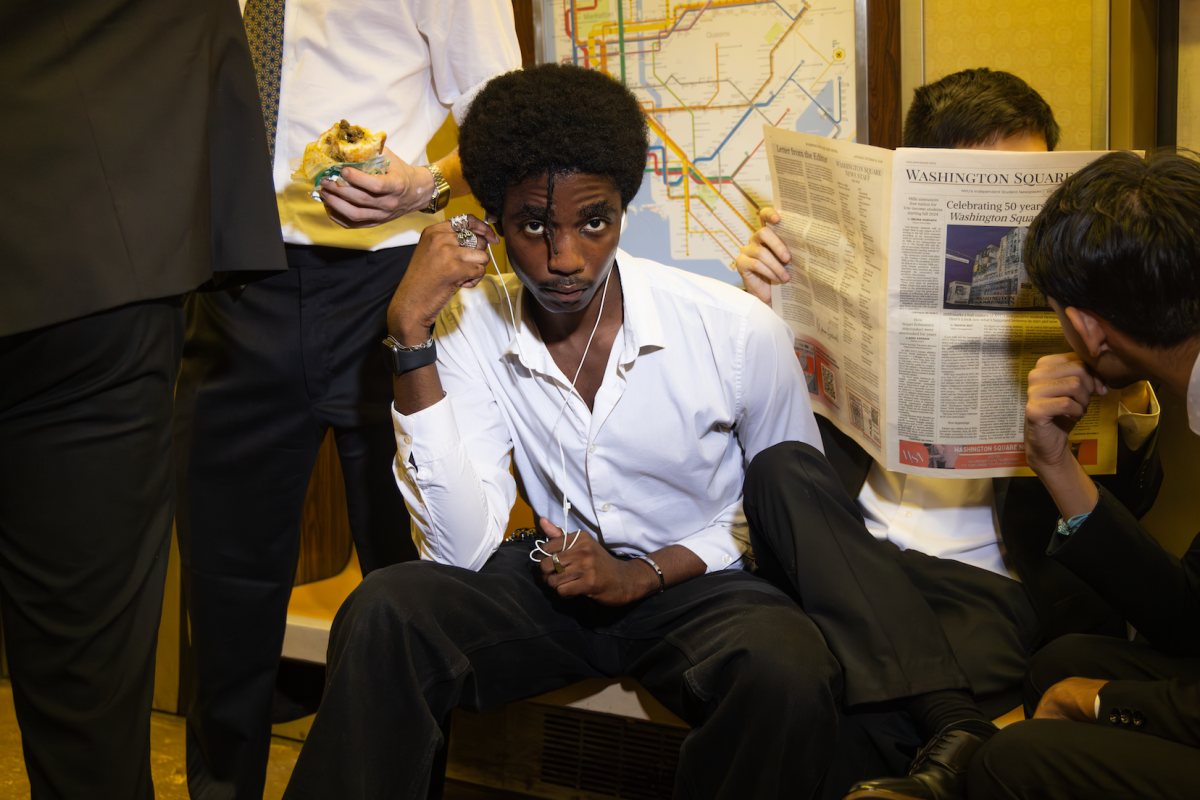
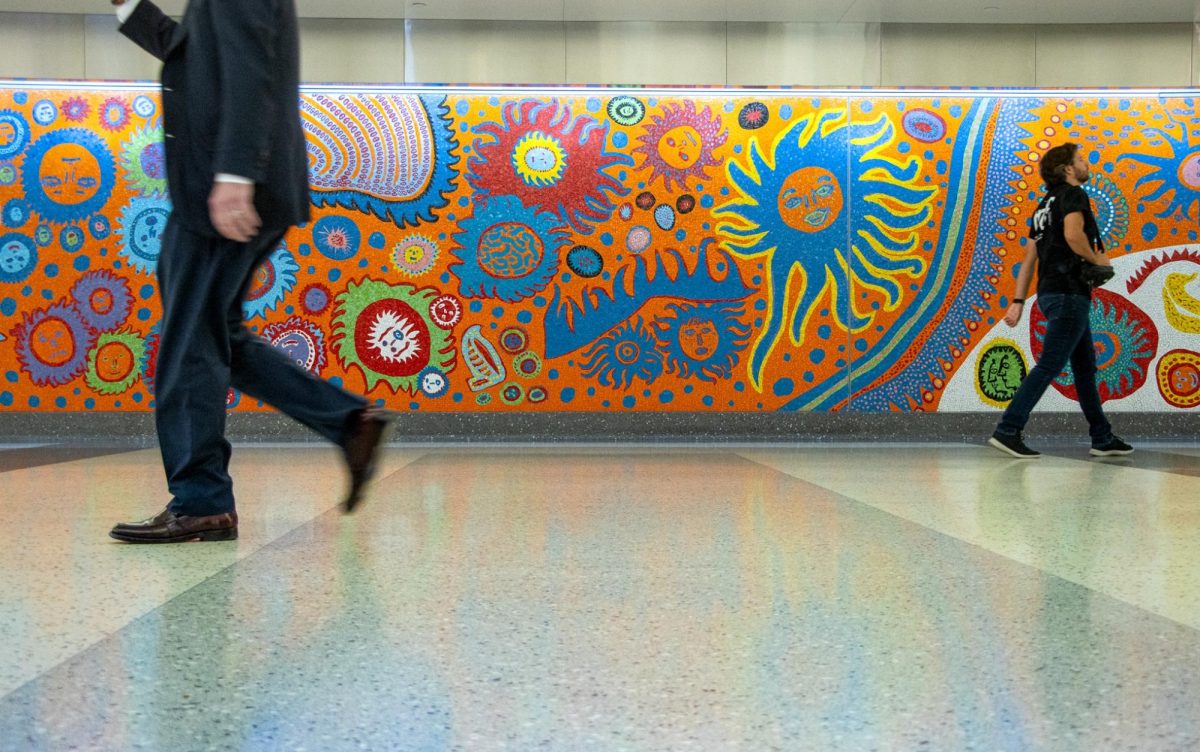
A study by NYU Rory Meyers College of Nursing found a correlation between COVID-19, sleep insufficiency and poor mental health among nurses. (Photo by Tony Wu)
February 11, 2022
Researchers from a NYU Rory Meyers College of Nursing study are calling for immediate action to support nurses during current and future pandemics. The group found increased rates of stress from inadequate sleep and exacerbated burnout due to shortened time between shifts and reduced work breaks.
Nurses from 18 states were interviewed and surveyed from June to August 2020, following the first wave of cases in the United States. Rory Meyers professors Lloyd Goldsamt and Victoria Vaughan Dickson participated in the study, as well as Lauren Ghazal, a postdoctoral research fellow at the University of Michigan.
“We felt that it was an opportunity to study the effects of the pandemic on nurses, and to sort of lay the historical record down of what was going on and document that in an empirical way,” Amy Witkoski Stimpfel, an assistant professor at Rory Meyers and the lead author of the study, said.
The findings showed 22% of nurses suffered from depressive symptoms, 52% from anxiety and 55% from insomnia. Sleep disturbances, including changes to shift schedules and a lack of work breaks, also contributed to deteriorating mental health among nurses. A series of 629 surveys and 34 interviews were conducted with nurses employed in healthcare settings.
“Our interviews with nurses were robust and throughout many of the interviews, participants became tearful and overcome with emotion,” Ghazal said. “There is so much rich data we gathered from these interviews.”
The study showed no direct relationship between inadequate psychological health and working directly with COVID-19 patients. Her research instead found evidence that the uncertainty of the early stages of the pandemic contributed to the study’s results.
“The nurses were sort of ruminating and replaying these events,” Stimpfel said. “They would either have difficulty falling asleep or they would wake up from a nightmare about it, not be able to go back to sleep, or wake up early and think about ‘Oh my gosh, I have to go back to work in a few hours.’”
The study followed research from a Workplace Health & Safety report, which found that nurses experience nearly twice the rate of depression compared to other professions. Ghazal’s study used the report to conclude that emotional support for nurses is needed outside of the workplace.
Rory Meyers junior Allison Rosen was not surprised by the study’s results since she has family members employed in healthcare settings. Her ideas about the profession and its psychological toll changed after watching media coverage of nurses and witnessing her roommate, a Rory Meyers senior, train in hospitals.
“I would be seeing articles with pictures of nurses and always just looking so defeated after seeing patients,” Rosen said. “It really did help me understand it — even though you’re helping people all the time. It’s not easy, emotionally, at all.”
Since starting her clinical rotations in fall 2021, Rosen has created a self-care routine to alleviate the stresses of her profession. She tries to maintain a consistent sleep schedule and prioritizes alone time to avoid burnout from the high-paced environment.
After conducting the study, the researchers developed strategies to help nurses combat stress from the pandemic. Ghazal encourages her students to utilize NYU’s counseling services and to not feel ashamed of seeking support. Stimpfel advises nursing students to talk with their employers about wellness support offered to their staff.
“There needs to be a multilevel effort here to protect, support and retain nurses,” Ghazal said. “We need to foster a work environment that allows nurses an autonomous practice, ensures adequate staffing and provides good compensation is key here.”
Ghazal said another study among the same group of nurses is underway. It will explore how nurses have managed stress after nearly two years of the pandemic, particularly with respect to increased vaccination rates and other factors.
Contact Maria Freyre at [email protected].