Langone researchers receive $470M grant to study long COVID
Long COVID-19 is a devastating chronic illness that may affect up to 37% of all patients, but very little research has been conducted on its symptoms and treatment. A new study at NYU Langone seeks to change that.
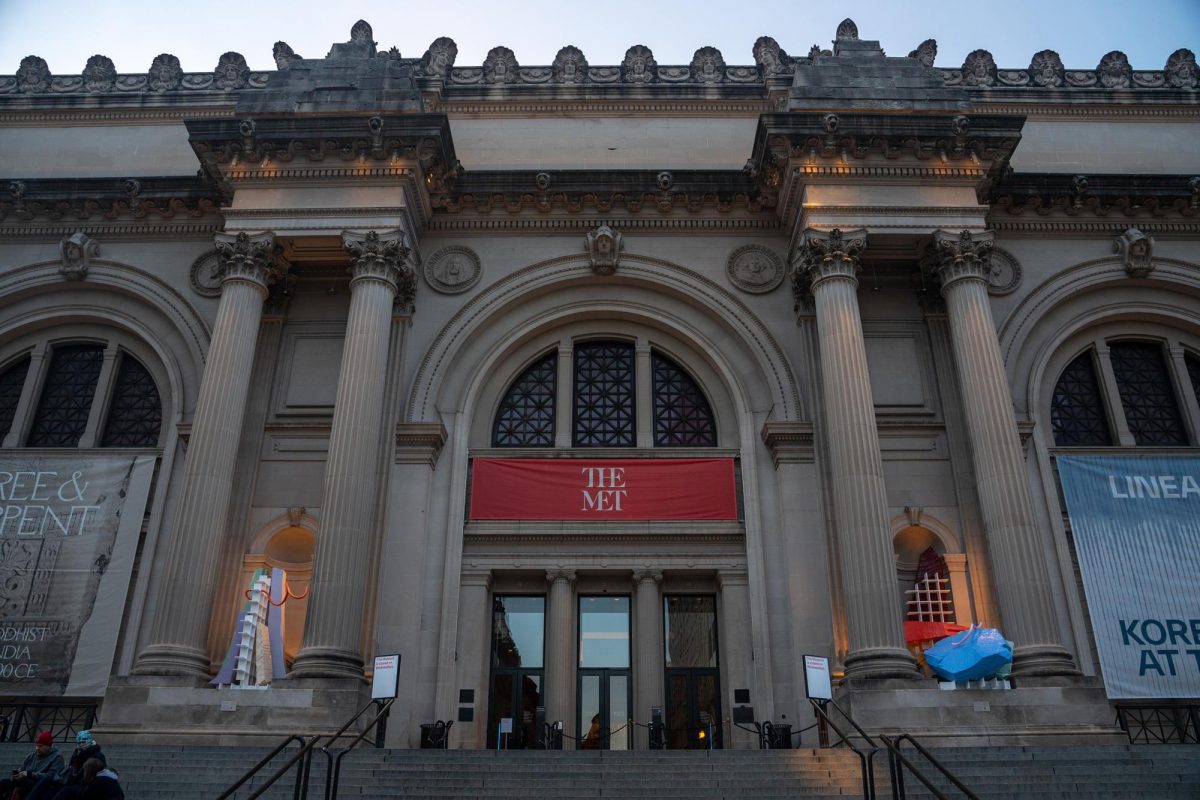
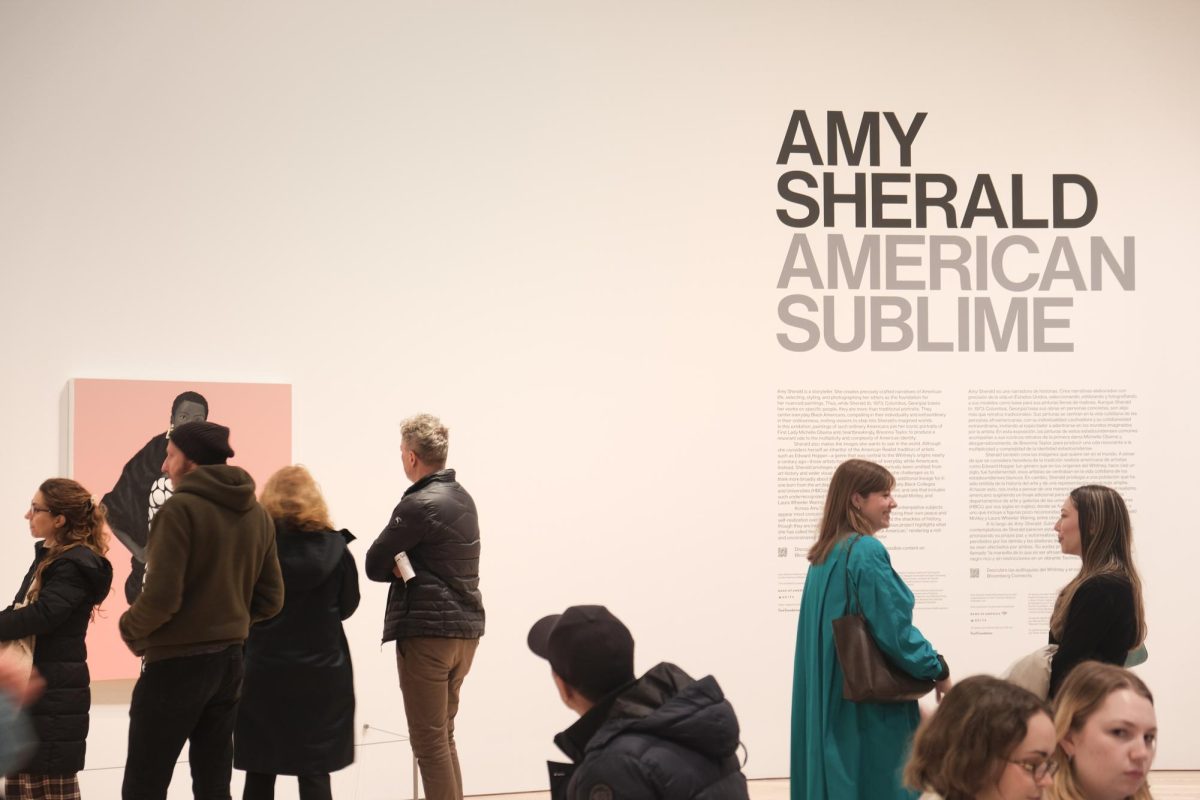
Months after being diagnosed with COVID-19, some patients are still experiencing side effects. Doctors at NYU Langone have been awarded $470 million from the National Institutes of Health to study long COVID-19. (Photo by Leo Shinegate)
October 25, 2021
Stuart D. Katz, a cardiologist at NYU Langone Health, tested positive for COVID-19 in December 2020. Months later, he still experiences symptoms and said he is only now starting to feel like himself once again.
“There are some things that haven’t returned to normal, which are disconcerting to say the least,” Katz said. “I still have a few lingering things that are sort of perplexing to me, even as a doctor and a researcher.”
Katz, the director of Langone’s heart failure program, hopes to integrate his experience with long COVID-19 — a term for the prolonged continuation of symptoms after a COVID-19 patient has tested negative — into his research. One recent study found that almost 37% of all COVID-19 patients experience long-term symptoms after the initial illness.
Along with colleagues Leora Horwitz and Andrea B. Troxel, Katz was awarded a $470 million grant by the National Institutes of Health to study long COVID-19 as part of the NIH’s REsearching COVID to Enhance Recovery, or RECOVER, initiative.
Katz, Horwitz, Troxel and other NIH researchers are currently recruiting participants for the study. The Langone researchers will conduct research on patients with long COVID-19, monitor enrollment and supervise the study in over 200 sites across the country. Patients can be of any age, but children, pregnant women and newborn infants are being sought out in particular. The long-term effects of COVID-19 have yet to be determined, since few large-scale studies have been conducted on the illness.
“The first goal of the study is to comprehensively characterize the features of long COVID-19,” Troxel wrote to WSN. “What is the range of symptoms, who is affected, how common is it and how long does it last?”
Steinhardt senior Haley Nemec was diagnosed with COVID-19 in early September despite being fully vaccinated. She visited the hospital numerous times, sometimes having to call an ambulance due to fatigue, brain fog, shortness of breath and chest pain. Nemec received multiple inconclusive chest X-rays. She will now be participating in the research at Langone.
“I feel pretty powerless,” Nemec said. “I hope researchers are able to find out a timeline of how long long COVID-19 actually is. I also hope they are able to find and create drugs and treatments that better mitigate long COVID-19 symptoms.”
“Long COVID-19 stops you … It isn’t just the first 14 days of testing positive. This can affect you and your health for months on end.” Haley Nemec
Since the onset of the pandemic, Langone has administered at least 26 other studies related to COVID-19, but most focused on the short-term effects of the disease. The researchers submitted a 300-page application in a three-week time frame — something Katz noted is extremely unusual for clinical research.
“The medical school has put in a lot of time, effort and strategic thinking about how to build a research infrastructure that could support these types of large studies,” Katz said. “It’s a whole team of people who are trained and ready who all came together in a moment’s notice. The highest leadership of the medical school said this is a high priority.”
The researchers have emphasized the importance of allowing patients and caregivers to influence how the study is conducted. They created a national patient engagement panel so that patients could provide direct input to the NIH.
“It’s a feature that is somewhat unique in this type of large multicenter research,” Katz said. “Hearing their stories is very compelling. So many patients were really not taken seriously by their health care providers. It’s a really important mess, and that’s part of our communications.”
However, some academics have raised doubts about the effectiveness of the RECOVER initiative’s patient inclusion strategies. Lisa McCorkell is a co-founder and patient-researcher at the Patient-Led Research Collaborative, a group of patients living with long COVID-19 who are conducting research on the illness. She worries that RECOVER is not taking patient feedback seriously.
“The protocols and inclusion criteria have not been made accessible for patients to comment on,” McCorkell said. “We have many concerns that could be addressed if we had the opportunity to review.”
The Patient-Led Research Collaborative applied to be part of the RECOVER initiative as a research partner but did not receive a sub-award — awards given to smaller research teams to help create the protocols with and conduct studies. The group, however, hopes to influence the study in other ways.
“We have been invited to the patient engagement calls and hope to have the opportunity to more meaningfully collaborate with the Langone team and RECOVER to ensure the study is helpful for people with long COVID-19 and people with related post-infectious illnesses,” she said.
Clinical research into chronic illnesses is sometimes controversial. In the past, studies have not been representative of the actual population with the disease or ailment being studied, according to Katz. Others have neglected to take into consideration the underlying causes behind a patient’s illness.
Sage Gustafson, a medical ethics researcher at NYU Langone, said she is cautious about most research related to post-viral infections, especially myalgic encephalomyelitis/chronic fatigue syndrome, which has similarities to long COVID-19. But she believes research into post-viral infections is desperately needed.
“I do think that the Department of Population Health at NYU does very excellent work,” she said. “I hope that these projects are designed in consultation with those who have long COVID-19, as well as those who have existing expertise on POTS [postural tachycardia syndrome], ME/CFS, fibromyalgia, and other conditions that seem to arise as post-viral sequelae.”
Katz added that the RECOVER initiative and Langone are dedicated to ensuring that the study sample represents the population of those who have long COVID-19 — primarily underrepresented groups.
“We’re recruiting everywhere,” Katz said. “The sites were selected by NIH, specifically with this eye towards sites that have long-established relationships with communities for recruitment of underrepresented minorities — the communities that have been highly impacted by COVID-19.”
After an initial questionnaire and the testing stage of the study, additional research will seek to determine what leads to the development of long COVID-19, its impacts on brain and body function, and who is most at risk. Clinical trials will then be conducted to find treatments for the condition.
Along with drugs and treatment, Gustafson believes that a diagnostic test for post-viral infections would be valuable for patients with long COVID-19.
“Ruling out anything else until all you’re left with is ‘nonspecific post-infection symptoms’ is a huge barrier to appropriate treatment and even a community,” Gustafson said. “There are equity issues in who gets diagnosed, who gets accommodations and who gets recognition, and a diagnostic tool would be a step toward alleviating those issues.”
Nemec hopes that everyone, especially young people, will take COVID-19 more seriously and realize that it could impact their lives after the initial infection.
“Long COVID-19 stops you,” Nemec said. “I have been unable to socialize, be self-functioning and independent, and I live in fear of going back to another emergency room. It isn’t just the first 14 days of testing positive. This can affect you and your health for months on end.”
A version of this story appeared in the Oct. 25, 2021, e-print edition. Contact Rachel Fadem at [email protected].