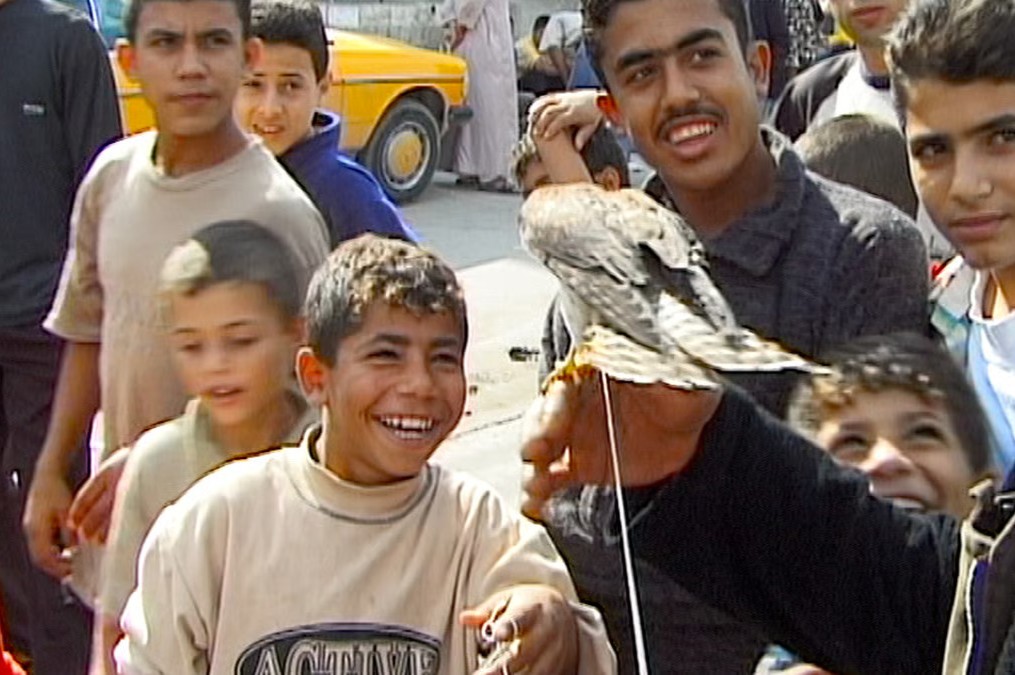
At the NYU-CUNY Prevention Research Center, researchers are changing the way immigrant and ethnic communities access healthcare by turning to health professionals that are not doctors, nurses or researchers. Rather, they are community members, called community health workers, who provide and translate essential medical knowledge to other residents while providing a sense of familiarity.
The CDC has recently granted the NYU-CUNY Prevention Research Center more than $3 million, which will be used to help provide healthcare to patients who have experienced problems in the justice system. This is the third time the CDC has awarded the money to the center since it first opened in 2009; each grant is intended to aid the work the researcher center does as well as community health workers affiliated with the center over a five-year cycle.
According to research director Dr. Nadia Islam, community health workers are crucial to the center’s work, as they build trust with patients who might otherwise be unsure of how to navigate the health system or are unable to do so due to language barriers.
Md. Jalal Uddin started working for the center as a community health worker in 2015, when the center began to focus on hypertension in ethnic communities. He works with Bangladeshi communities by translating medical information for patients to understand and manage their hypertension. He also holds motivational interviews and information sessions to help patients figure out how they can change their lifestyle to improve their condition.
“Doctors provide medicine, but not only medicine helps to lower or manage [patients’] uncontrolled blood pressure or diabetes,” Uddin said. “So there are other things also which need to be implemented or done.”
Islam explained that without the community health workers, a well-researched and developed program is only as impactful as it is accessible to its patients.
“You might have a great program that doesn’t work very well in a very under-resourced, too-busy primary care clinic,” Islam said. “Or you might have a great program that was tested rigorously, but doesn’t really consider a kind of political and cultural environment that it is being implemented in.”
Implementing a program to better suit a certain community can be as simple as translating it into a language that is more accessible or providing meal planning that takes a culture’s dietary restrictions into consideration.
The center used the last cycle of CDC funding — granted in 2014 — to focus on reducing high blood pressure and improving cardiovascular health in South Asian communities. It uses the community health worker model to implement programs in primary care centers around the city. These programs guide patients on how to adequately manage health problems beyond just taking medicine prescribed by doctors.
The research center also evaluates how to improve practices of primary care centers to better serve patients. The center has taught primary care centers how to better utilize electronic record systems to identify patients with patterns of high blood pressure. Doing so alerts physicians which patients may benefit from additional health advice, according to Islam.
Community health workers like Uddin can use this information to call and encourage patients to attend informational workshops and discuss ways of managing their health. According to Uddin, patients are usually receptive to his calls and are eager to have access to more resources.
In 2009, Islam and the current co-principal investigator for the center, Dr. Chau Trinh-Shevrin, were conducting research on health disparities within immigrant communities in New York when they applied for funding from the CDC. The money allowed them to develop the center’s infrastructure so that they could not only conduct research but also disseminate their findings into care centers and even create policy briefs — known as white papers — based on their findings. They’ve developed a white paper about integrating community health workers.
“What our center infrastructure enabled us to do was bring together experts and stakeholders from across the country to be able to inform that white paper,” Islam said.
While the research center focuses on New York City, their findings do have a national application.
“Our prevention research center is important because it serves as a hub for innovation on sustainable and scalable policies and programs to address health inequities both in New York City and nationally,” Dr. Anna Divney, a CUNY senior research associate with the center, told WSN via email.
Although the center has focused on different health issues and communities, it is guided by a singular idea.
“A real common theme in our work is to really understand the context that communities are coming from and to shape programs that really work for them,” Islam said.
A version of this article appeared in the Monday, April 1 print edition. Email Bethany Marie Allard at [email protected]