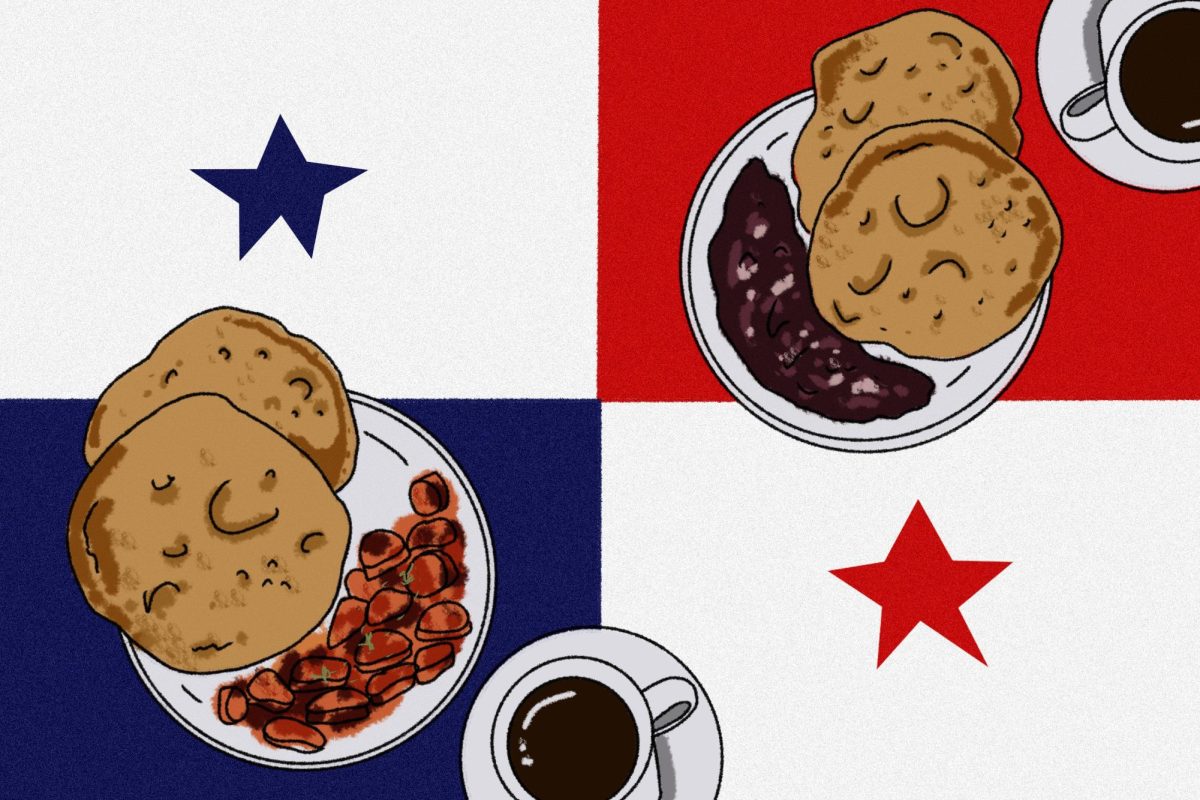
Langone Pioneers ‘Death Masks’ for Deceased Facial Donors

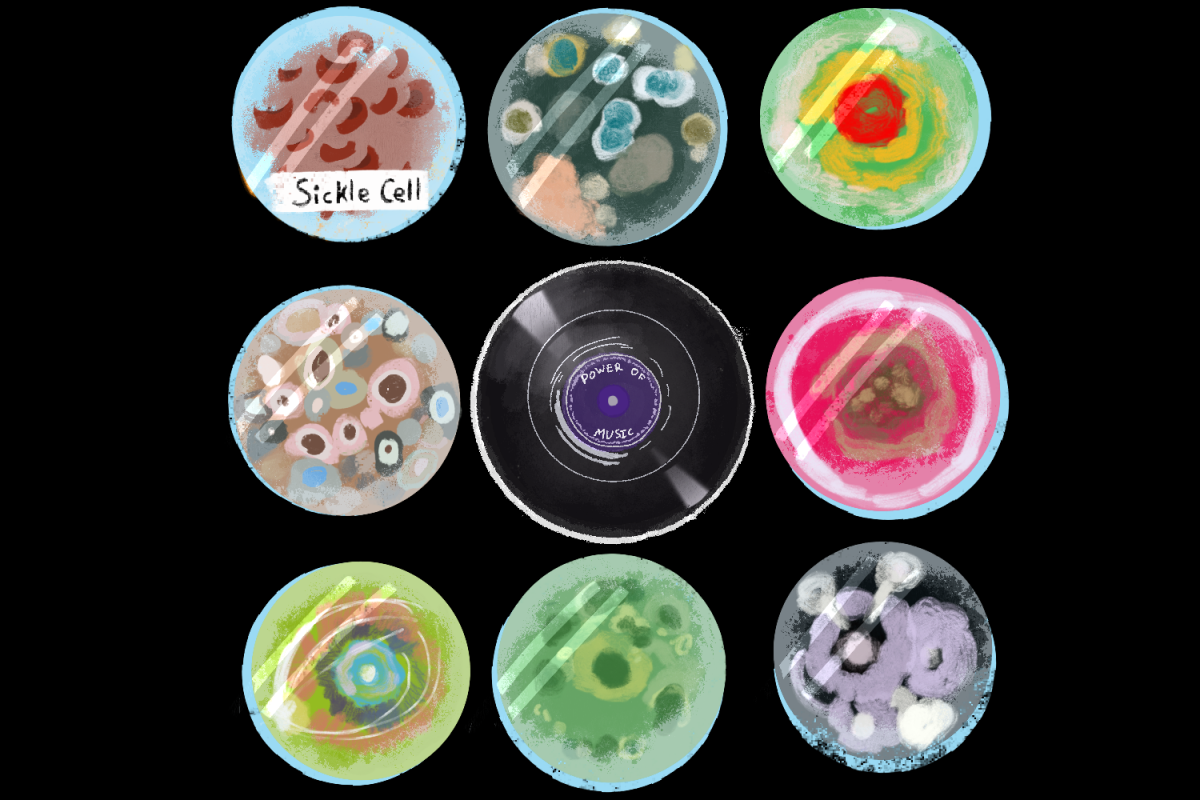
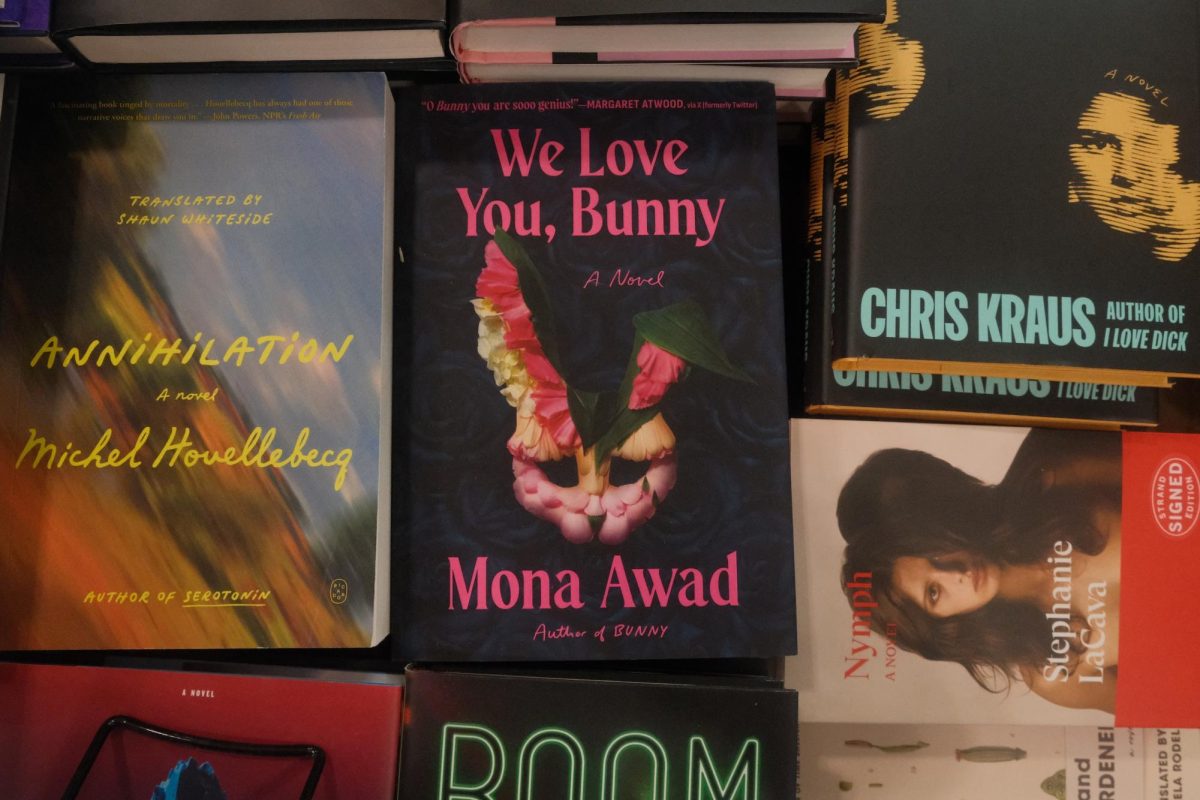
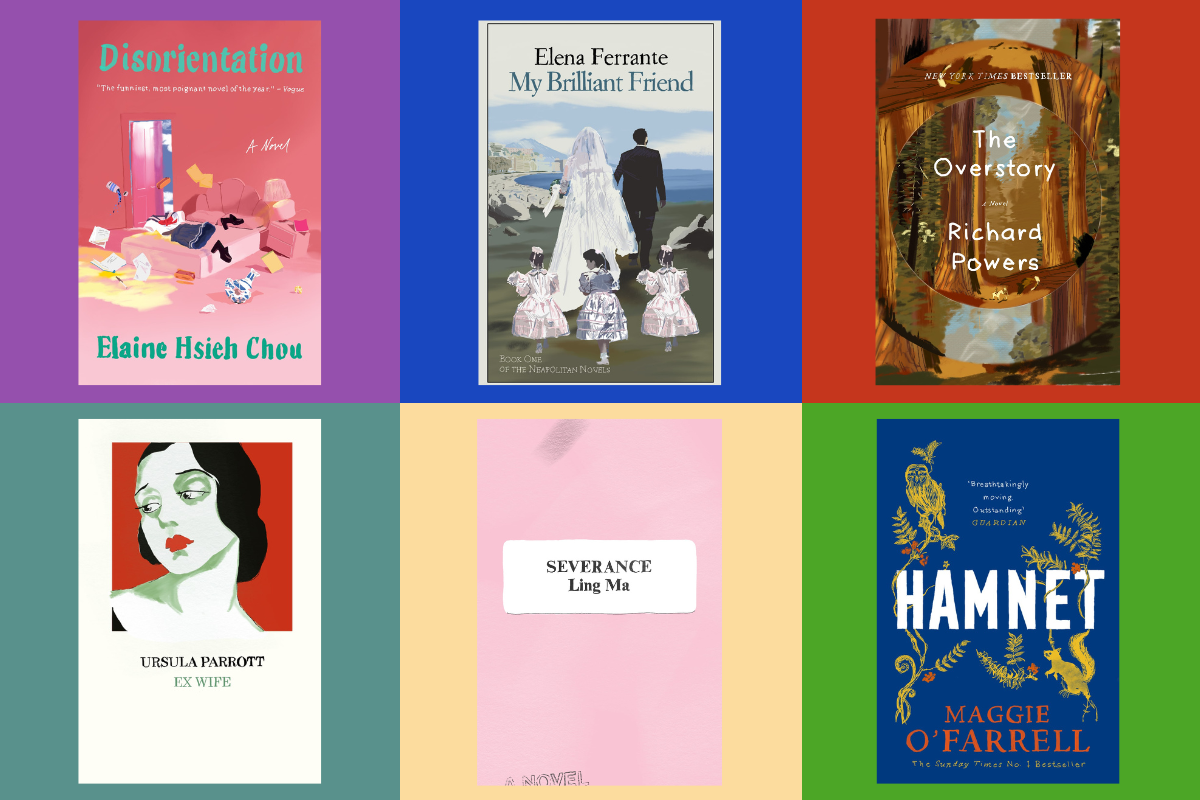
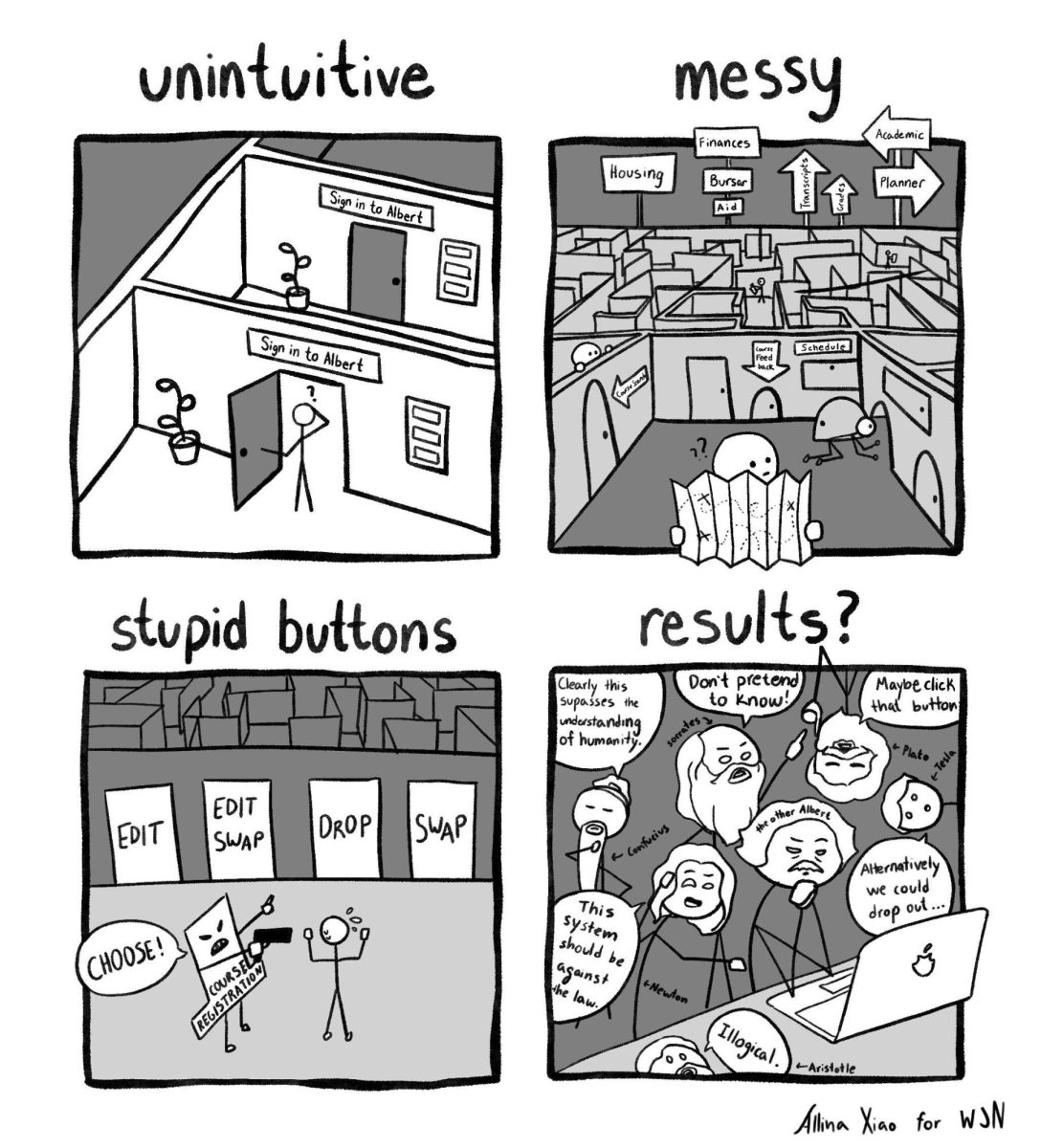
Courtesy of NYU LaGuardia Studio
A sample mask, featuring Leslie Bernstein, administrator for the Hansjӧrg Wyss Department of Plastic Surgery and Face Transplant Program at NYU Langone Health.
January 23, 2018
In 2001, Mississippi volunteer firefighter Patrick Hardison was severely burned and disfigured when the roof of a burning building collapsed onto him. His eyelids, ears, lips and nose were completely destroyed, leaving no normal tissue on his face.
For almost 15 years, Hardison lived in constant pain — unable to blink, eat or form facial expressions normally. Everytime he left the house, people stared; children ran away. Activities like driving and swimming, which he had enjoyed before the accident, were suddenly out of the question.
But in 2015, after a tragic accident, 26-year-old David Rodebaugh helped give Hardison a normal life again.
The family of Rodebaugh, who died in a biking accident, agreed to donate his face, which was a perfect match for Hardison. In August 2015, a team of NYU Langone Medical Center surgeons, led by Dr. Eduardo Rodriguez, performed the most extensive face transplant surgery on record.
After several revision surgeries, Hardison learned how to talk and swallow again. Eventually, thanks to his new eyelids, he was able to drive again. And in 2016, he was back to living a normal life.
Hardison’s experience is unique for many reasons. One of which is the unlikelihood of receiving a donation like he did. Even for registered organ donors, families still have to give approval before a face is removed for transplant. While Rodebaugh’s family was willing, the idea of removing a loved one’s face post-mortem is too much to ask for many.
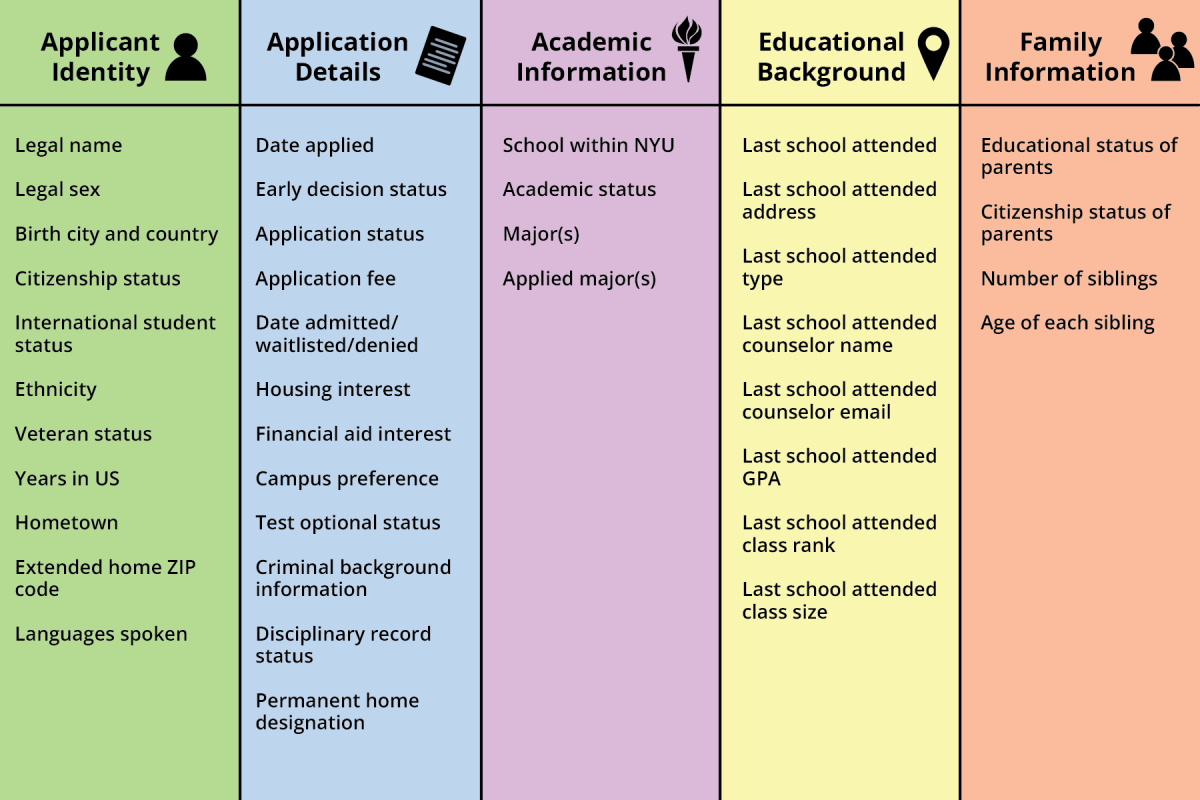
Current replacement masks for deceased face donors are made of hard silicone and are only 75 percent accurate to the face they are replacing.
“Typically a mold is taken of the donor’s face that is filled with silicone to create the mask, which is then hand painted,” said Rodriguez, chair of the Department of Plastic Surgery at Langone. “The silicone masks we use today are archaic.”
Rodriguez is seeking to change that.
Using 3-D imaging and printing technology, he plans to make a high resolution scan of the donor’s face will be taken with a handheld camera in the hospital. The image will be retouched and printed in full color at the LaGuardia Studio.
The mask, which takes approximately 30 hours to create, will be 95 percent accurate to the flesh and blood face of the donor.
“I wanted to develop a more accurate replica mask of the donor with a shorter production time,” Rodriguez said.
Only 37 face transplants have been performed worldwide — the number remains low partly due to the difficulty of finding a compatible candidate for transplant.
“The search requires a blood, antibody, skin tone, hair color and facial bone structure match — an exacting process that limits the potential number of viable donors,” Rodriguez said.
Langone currently has another patient waiting for a face transplant procedure, and Rodriguez hopes that the 3-D printed masks will expand the small pool of donors available.
“We think these new incredibly lifelike masks could potentially bring about more donors, enabling us to more quickly care for a greater number of face transplant patients,” Rodriguez said.
Email Sakshi Venkatraman at [email protected].