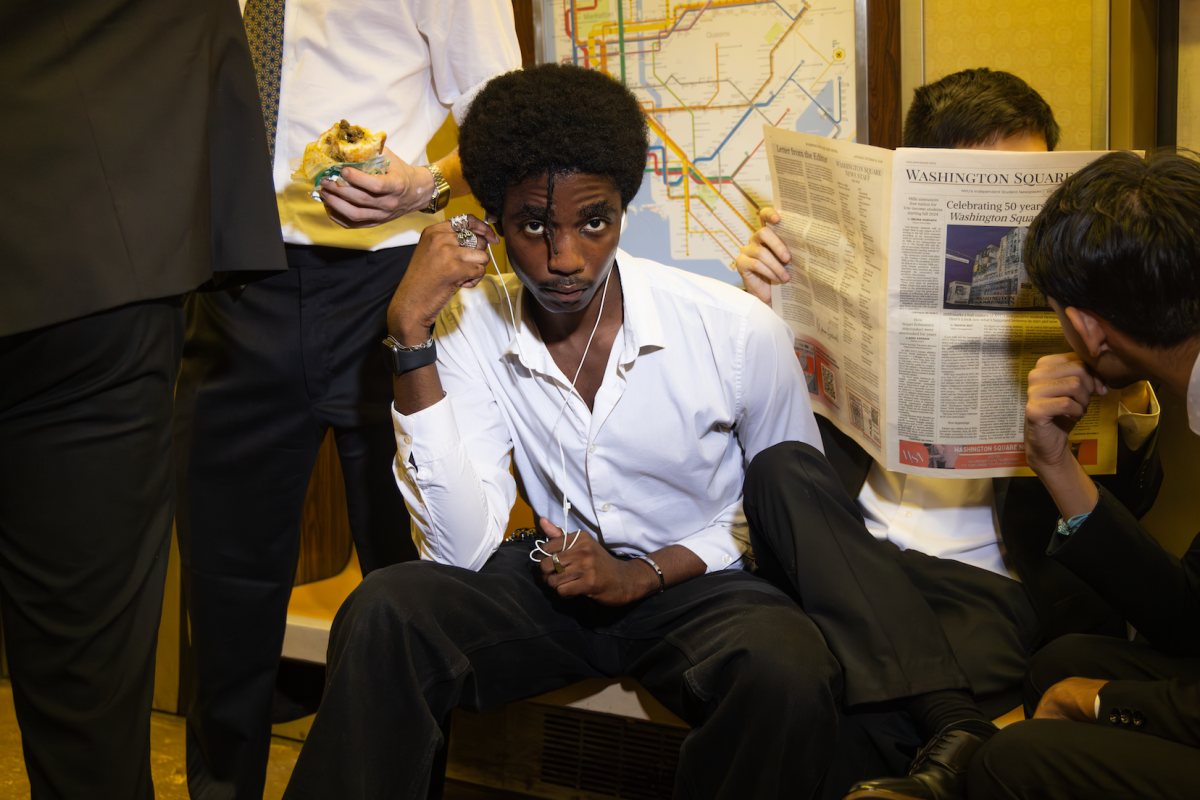
Dr. Leigh Charvet Strives Towards MS Treatment
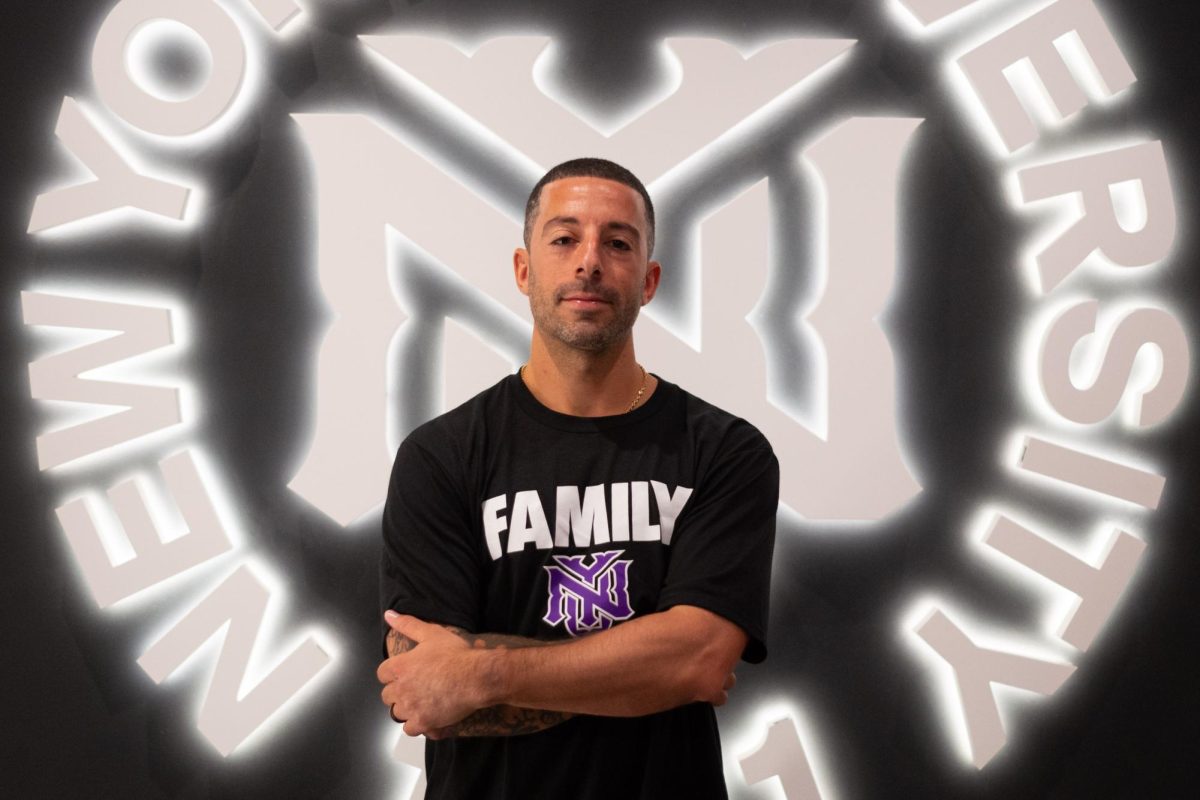
Dr. Leigh Charvet, an associate professor of neurology at NYU’s Langone School of Medicine. Dr Charvet collaborated with recent NYU graduates to develop a painless treatment for everyday symptoms of Multiple Sclerosis that patients can use from home.
February 27, 2017
The research of NYU School of Medicine’s Dr. Leigh Chavret is facilitating advances in the development for treatments for Multiple Sclerosis.
Charvet, an associate professor of neurology, collaborated with recent NYU graduates Bryan Dobbs, William Pau, Natalie Pawlak, Ashley Clayton, Michael Shaw and Kai Sherman to develop a painless treatment for day-to-day symptoms of MS that patients can use from home.
The remedy involves transcranial direct current stimulation, which delivers low amplitude electrical currents through scalp electrodes. CUNY professor Marom Bikson and Abhishek Datta of Soterix Medical collaborated with the research group to engineer a custom-made, remotely controlled tDCS headset for the study.
The headset allowed Charvet and her research team to video conference with patients, complete safety checks and administer preprogrammed doses remotely. Their findings were originally published in the February edition of the medical magazine Neuromodulation: Technology at the Neural Interface.
Charvet said her research was inspired by the fact that regular MS treatment deals with the decline and relapse of the disease but does not address patients’ debilitating daily pain. The field of neuropsychology is concerned with this symptomatic management that she discovered as an undergraduate student at the University of Michigan.
“I got a job in the physical medicine rehabilitation unit, working with neuropsychologists,” Charvet said. “That experience set [me] on this path for life for how you can merge medicine with the principles of psychology and focus on seeing the patients as full,
rich individual[s].”
Charvet’s interest in neuropsychology led to her research at Stony Brook University with neuropsychology professor Lauren Krupp, where they found that cognitive remediation computer games — when played at home and remotely supervised — helped alleviate cognitive symptoms of MS. After realizing the desire of patients to receive clinical treatment at home, Charvet worked to combine remote-access clinical treatment with tDCS research, which has positive rehabilitation benefits for cognitive disorders.
“MS is a fascinating disorder, and you just want to do everything you can to help,” Charvet said. “It just really drives you to see what you can do to predict [and] where we can intervene to help.”
Charvet also said that tDCS treatment is not disorder-specific, so it can help treat a variety of disorders with similar cognitive symptoms to MS — including attention deficit hyperactivity disorder, depression and Parkinson’s Disease. Parkinson’s is presently the subject of a new tDCS clinical trial. However, Charvet’s study marked one of the few tDCS studies to have a 20-session treatment period, enabled by its remote supervision format. Charvet said that more research must be conducted before tDCS is clinically available but that this study still marks progress in understanding the applications of tDCS.
“We’re really at the tip of the iceberg of understanding it,” Charvet said. “It’s very exciting and there’s a lot of promise. [tDCS] definitely does something, and we’re just trying to harness and understand what it does.”
A version of this article appeared in the Monday, Feb. 27th print edition. Email Caroline Haskins at [email protected]