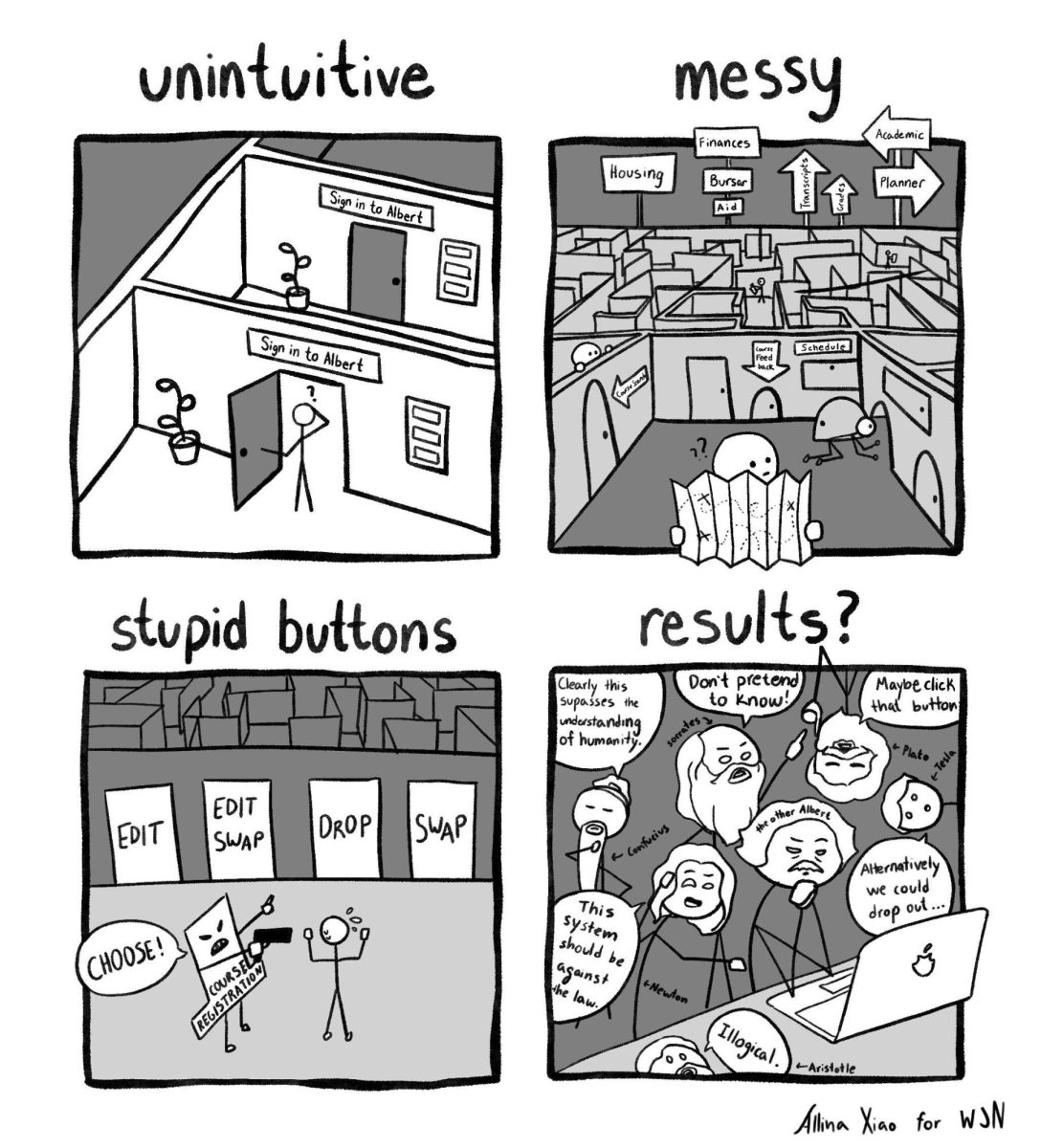
Panel discusses ethics of experimental drugs
Arthur Caplan discusses legal issues surrounding euthanasia.
February 4, 2015
NYU Langone professor Arthur Caplan led a discussion on Wednesday at NYU Law about the ethical use of experimental drugs for terminally ill patients.
Arthur Caplan, who is a member of the NYU Working Group for Compassionate Use, began the event speaking about Josh Hardy, a child from Virginia who suffers from a life-threatening kidney disease. Hardy’s family sought a drug in development that showed potential for treating Hardy’s viral infection. Chimerix, the company that manufactures the drug, denied two requests to release it from St. Jude’s Children’s Hospital, but eventually capitulated due to pressure from a social media campaign.
Caplan explained that the drugs rarely make it from animal trials to pharmacy.
“When somebody says, ‘I want it,’ there’s a pretty good chance that it isn’t going to work,” Caplan said. “If it was easier to do this, we wouldn’t have so many diseases that we wouldn’t be able to cure.”
NYU Law student and co-president of the Health and Law Policy Society Isaac Ritter, who coordinated the event, said the compassionate use discussion is significant.
“This is all more acute in the age of social media, where campaigns can catch fire, pressuring stakeholders to provide experimental drugs to patients,” Ritter said. “While these efforts are well-intentioned, they pose serious risks and ethical concerns we must address.”
Caplan added that there is a lot of uncertainty when it comes to the legal process of experimental euthanasia drugs. Some people are reluctant to move forward because it is currently illegal.
Caplan also discussed the difficulties in dealing with minors, hospice patients and disabled, non-terminally ill people who also want access to drugs.
“I don’t think right-to-try laws will result in any access,” Caplan said. “I would expect all 50 states to pass them by the end of this year.”
For steps to improve compassionate use, Caplan argued for improved awareness of the issue, independent vetting of drug requests, reporting of all treatment outcomes to the FDA and addressing payment issues.
Ashley Ferguson, another co-president of the Health and Law Policy Society, emphasized the importance of the debate.
“The way that health law is right now, so much of what we hear is coming from the other side,” Ferguson said. “Even though they know the potential for complete failure of medicine, if they are willing to try, we should also be willing to try.”
A version of this article appeared in the Thursday, Feb. 5 print edition. Email Jimmy Chin at [email protected].